We miss our Lukas and so often wish we could be sharing life’s journey with him. The next best thing is continuing to honor his memory with Lukas' Fund, and by sharing his story with you. The goal of the fund is to help the infants in the NICU and their parents, in particular the NICUs at Athens Regional Medical Center in Athens, Georgia and Grady Memorial Hospital in Atlanta where Lukas spent his life.
11/15/02
| Born 11/15/02 Weight: 1 lb, 7.2 oz (659 grams) Length: 13 inches (33 cm) Gestational age: 31 weeks |
Mark H. Ebell MD, MS Laura L. Bierema EdD Athens, Georgia |
Please join us in welcoming Lu kas Willem Bierema Ebell to our family.That's right - he couldn't wait to join us! A non-stress test showed a flat heart tracing, with little variability. That led to an ultrasound on Friday afternoon, which showed that Lukas had no fluid around him, and had actually stopped growing a few weeks ago.
kas Willem Bierema Ebell to our family.That's right - he couldn't wait to join us! A non-stress test showed a flat heart tracing, with little variability. That led to an ultrasound on Friday afternoon, which showed that Lukas had no fluid around him, and had actually stopped growing a few weeks ago.
There wasn't any choice - he had to come out, and only had hours or days to live in utero. After an urgent C-section, he was born kicking and screaming at 4:52 pm, with Apgars of 9 and 9, but only weighing 659 grams (1 pound, 7.2 ounces). Although very small, about the size of a 25 week old, he has the maturity and reflexes of a 31 week old. (For you medicos on the list, he had severe oligohydramnios and intra uterine growth retardation).
As you can imagine, this is a very difficult time for us, and there will be many ups and downs in the coming weeks and months. We're going to do our best to keep this site up-to-date so you can follow Lukas' progress with us. We look forward to your thoughts, love, and support.
11/16/02

All things considered, Lukas is doing great. He has never required a ventilator, and at 12 hours was breathing room air. He is now (25 hours of age) getting a little oxygen again so he doesn't have to work quite so hard. His initial chest x-rays, heart echocardiogram, and brain ultrasound today were all normal, and he remains vigorous. He is beginning to suck on his tiny little pacifier, grasps at our finger, and responds to our touch. He is truly precious, and we love him very much.
Although tired and sore, Laura is doing well. She was up in a wheelchair within a few hours of surgery to visit Lukas in the neonatal intensive care unit (NICU), and the next morning was already walking 20 yards down the hall to the NICU. She is a trooper, but needs her rest over the next couple of days. Both sets of grandparents are arriving from Michigan (Bieremas) and Florida (Ebells) tomorrow afternoon, and we look forward to seeing them.
11/17/02
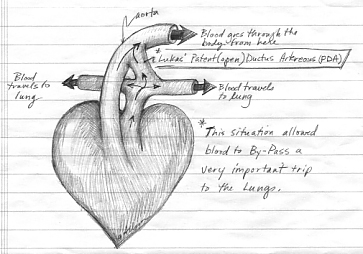
Lukas had to go back on his oxygen today, and received one blood transfusion and two platelet transfusions. His umbilical artery catheter had to come out, and he is getting an arterial line as I write this (10 pm). Otherwise, he is doing fine. There is a small patent ductus arteriosus, which means that there is a connection between the arteries that supply the lungs and the rest of the body. This makes it a bit harder for him to oxygenate, and if it doesn't close on its own by tomorrow, he may have to have a procedure to close it via catheter. It can sometimes be done with medication only, but his platelet count is low, and his neonatologist hesitates to use the medicine (indomethacin) for that reason. We'll see tomorrow.
 As you can see from the photos, Laura got to hold Lukas for the first time today. He melted our hearts - it was important for all of us to have a chance for some real contact. We hope this becomes more frequent as he gets stronger.
As you can see from the photos, Laura got to hold Lukas for the first time today. He melted our hearts - it was important for all of us to have a chance for some real contact. We hope this becomes more frequent as he gets stronger.
Speaking of the neonatologist, she is terrific. Dr. Faase is Dutch, and grew up about 20 miles from where my mother's family lives in Aachen. She learned her trade in Munich, so we think she is the perfect person to take care of young Lukas Willem. We all deal with things differently - I tend to intellectualize. Because I am afraid of flying, I know every detail of every plane out there, including how often they crash, the best and worst airlines, where to sit, etc. With Lukas, I deal with my fears in the same way. I went home and consulted the Cochrane Library, which contains the Oxford Perinatal Database, and is part of our software. I printed an "evidence report" on preterm birth and several other related topics, then read each of about 150 summaries. I identified about 10 key things that I thought the neonatologist should and shouldn't be doing. She was ten for ten, and knew her studies and evidence cold. Needless to say, I sleep better now.
11/18/02
The news is mixed today on our little buddy Lukas. The ultrasound test of his heart showed that his patent ductus arteriosus (PDA) appears to have closed. While the final report is pending, this is encouraging. Unfortunately, he has had increasing trouble maintaining a high enough blood pressure, and is also having trouble getting rid of his carbon dioxide (CO2). That led to some additional lines for monitoring and medication, the need for quite a bit of dopamine (20 mcg/min), and the need to be put on a ventilator for a while. We hope this is only a short-term need, but we'll see. The cause is unclear - maybe just prematurity, maybe infection. He is being treated for infection with 3 antibiotics, and other tests are pending. He also had some bleeding into his lungs, and we are having another scan of his brain tomorrow morning to make sure that he didn't also bleed there (there is an association between the two). On the bright side, his blood count remained good throughout the day, and his other labs look OK, and he is only on 40% oxygen on the vent. Laura still has her headache, but is gaining strength, and still hopes to go home tomorrow. Damn spinal! The epidural blood patch didn't work.
11/19/02
Lukas had a better day today. He came off the dopamine overnight, which was being used to keep his blood pressure up. The ventilator settings were reduced somewhat during the day as he needed less help, but then had to be upped a bit later in the day. Overall, better than yesterday... We had great news in that his cranial ultrasound was read (preliminarily) as normal. We had been concerned about a bleed, so learning it was normal was probably the best news I've ever heard in my life. I hope that there is more good news in the future.
Laura finally felt better today - her spinal headache went away in the afternoon, although the lack of pain in her head means she was more aware of the pain elsewhere. Overall, better, though. She went home this afternoon, and we had a nice dinner with our parents. It's good to be home, although we wish Lukas could have joined us tonight.
The staff have been terrific - every nurse in the NICU has taken lots of time to patiently explain how Lukas is doing, and they are incredibly attentive. It's hard to imagine a more difficult job, and they do it with wonderful grace.
11/20/2
Lukas had trouble maintaining oxygen levels on the ventilator, and is being transferred to Grady Memorial. It is a big, scary place in downtown Atlanta, 10 stories tall, but has one of the top NICUs in the state. Affiliated with Emory University, they have the equipment and sub-subspecialists that Lukas needs right now. On arrival, we first sat for an hour in the waiting room before they realized we were there. Dr. Dudell is very nice, and has a great reputation around the unit. There are students and residents around - it is a teaching hospital - which is different from ARMC.
Lukas is now on a high frequency oscillating ventillator. Picture your child vibrating at about 300 beats per minute while attached a blender that is pulsing air into his lungs. Sounds horrible, but is actually much easier on his lungs than the traditional ventilator. He was initially started on fairly high settings. The doctors were concerned about the amount of fluid that had accumulated in his belly, which could be caused by a variety of reasons. One concern was infection caused by a hole in the intestines, but that didn't appear to have happened (fluid drawn from the belly was clear and had no bacteria or white blood cells). The cardiac echo showed that the pesky ductus arteriorus was open (after apparently having closed) and could be contributing to his problems. If it doesn't close, he will require ligation of the ductus. This involves opening his little chest, all 6 square inches of it, finding the tiny 2 mm ductus, and tying it off, then closing him up. Although done in the ICU rather than the operating room, it is still a terrifying prospect for us.
The great news was that Lukas responded really well when they gave him some surfactant. He almost immediately required less oxygen and lower ventilator settings (i.e. it didn't have to do as much work for him). What is surfactant? It's stuff that your lungs make to keep the air sacs and airways flexible, and does other good things for the airway as well. The initial studies were done at UM while I was an intern. I remember they would put drapes around the incubator and play Beach Boys music (get it? Surfin' Safari?) to mask the rest of the folks in the nursery from whether the infant was getting surfactant (Exosurf) or placebo.The stuff works, and along with the high frequency oscillator has revolutionized care of these fragile young kids with breathing problems.
11/21/2

Good news this morning. His neonatologist was "very surprised" at how well Lukas did overnight, with much improved breathing, and requriing about half the support that he had needed when he came in. His liver and kidneys were working fine, and his blood counts were holding their own.
More good news with the cardiac echo. His PDA was smaller now (from "moderate" to "small to moderate") and the pediatric cardiologist did not recommend surgery at this point. He will repeat the study on Monday, or sooner if Lukas has a turn for the worse.
All the cultures came back and were negative, meaning that no bacteria grew from any of the specimens that they drew while Lukas was in Athens. The transfer note from the neonatologist in Athens referred to a small placental size, which could explain why Lukas stopped growing in the womb. The cause of the small placenta is uncertain, and we are trying to get the full report faxed over to us.
We are slowly figuring our way out around here. It's a big place, but the people are friendly and the staff at the NICU has been terrific. They let us basically camp at his bedside, and we have been here for about 12 hours so far today (it is 9 pm), leaving only for dinner. The hotel is spartan but clean and safe and closeby, and we figured out where there are a few restaurants that don't feature a clown or chihuahua in their advertisements. It looks like we will probably be here well into next week, and at best won't return to Athens till Thanksgiving.
11/22/2
Lukas was doing OK again this morning. The plan today is for the geneticist to stop by and examine him, cardiology to repeat the echo to check on the patent ductus arteriosus (PDA), and continue to wean him from the high frequency oscillating ventilator. We ran to Athens to get clothes and books for a week's stay, which is what we are now looking at - minimum - in Atlanta.
The geneticist said that Lukas looks like what we think he is - a beautiful little boy, with the emphasis on little. No changes that suggest a chromosomal problem, although the final answer will be in the karyotype, and that will be at least another week. We tried the wean, but it didn't take. After about 45 minutes his pCO2 (carbon dioxide) was 85, much too high, and he had to go back on the vent. He did fine back on the "hi fi" vent, and rested well overnight.
11/23/2
Lukas had a fairly quiet day today, with one exception. He was placed on his stomach for a change of position, and drooled quite a bit (or as they say down here, a good little bit). This loosened the adhesive on the tape holding his breathing tube (connected to the ventilator) in place, and it slipped out a bit. In trying to fix it , it slipped even more, and had to be pulled out all the way and reinserted. Scary time - lots of running around, bagging him, and so on, but he tolerated it extremely well and was back to par within a few minutes. During the day he gradually came down a bit more on his settings, and rested quietly. They are doing some studies on his bowels now, running some barium through them to make sure they are working and intact. Should have that answer tomorrow or Monday. The PDA was a bit smaller today, which is encouraging, but may still require repair. The echo will be repeated Monday and I suspect that may be the final test before deciding to repair or not repair.
Laura's feeling better - we found a nice Thai restaurant in the Virginia Highland neighborhood (Surin of Thailand), and went there last night and tonight. Tomorrow, Italian. Our typical day here is:
- gourmet continental breakfast at the Comfort Inn
- get to the hospital around 9 am
- spend the day there - Mark delivers lunch from the hospital cafeteria, as it is too far of a hike for the still recovering Laura
- dinner out (our break for the day)
- a check-in visit after dinner with Lukas
- back to the hotel around 10:30 pm or so
It is wonderful that we have the flexibility and support from our families to allow us to be here. Thank you!
Our good friend George Seifert flew down from Michigan Friday, and spent last night and today with us. How wonderful - it was a comfort to have him here. He is a family physician in Marshall, Michigan, and I went to college, med school, and residency with George. We have traveled all over the world together (I've probably logged more miles with him and Jim Boyd than anyone but Laura!), and we both very much appreciate his visit. He'll spend tomorrow with us before flying back home. Thanks for Sheri, Britta, and Anna for doing without their Dad for the weekend, especially since little Anna was starring in "The King and I" and it premiered Friday!
11/24/2
Below are some photos taken today with our friend George (left) and Laura's parents Ken and Phyllis. We wanted to minimize the number of flash photos and disturbance of our little guy, so I'm stuck looking constipated instead of getting a chance at another photo. Oh well. Phyllis is holding her hand up to compare it with Lukas (yup, he's in there somewhere under all those tubes!).

Today was pretty quiet - not much typically happens on Sundays, and today Lukas just spent the day gradually 'dialing down' the settings on his respirator. His labs remained fine, and the barium continued to work its way through his gut, making it unlikely that he has an obstruction of his bowel (a good thing). It was great seeing Ken, Phyllis, and George, and we very much appreciate their effort in coming to visit. Tomorrow promises to be a busy day, with another ultrasound, and possibly another attempt at weaning or even an attempt at correction of the ductus arteriosus. We're going to try to get a good night's rest.

11/25/2
When we arrived, Lukas was on about the same ventilator settings as the night before. The upper half of his belly, especially on the left, looked a little bluish, which is caused by some build-up of bilirubin in the liver. His skin is so thin that we can see the liver right through it. The pediatric gastroenterologist saw him today, and wasn't alarmed by that. He ordered some tests, but hopefully this is just a matter of his gut being slow to get moving due to the prematurity. Some x-rays of his abdomen show that the bowel appears open (contrast is inching through it), although it is working very slowly. The pediatric surgeon saw him just to get to know him, and in case any surgery is needed (none is planned for now). The fact that the bowel appears open and unobstructed will hopefully make his skills unnecessary. Finally, the pediatric cardiologists came back and did another echocardiogram. It shows that the ductus is larger than ever, and will definitely require closing. Although we had hoped it would close, at least we have a possible explanation for a lot of his problems, since this large ductus could cause the bowel and breathing problems that he has been experiencing. The decision was made fairly late in the day, so Lukas is going to rest up tonight and get a new arterial line tomorrow morning (this allows continuous monitoring of blood pressure and blood gas monitoring without poking him, both of which will be needed for the surgery and beyond). Hopefully the surgery will happen tomorrow so we can all put it behind us. Fortunately, Laura is feeling better - no headache today after 10 days of spinal headache - and is getting more mobile.
The staff have been great, and we are getting to know some quite well. One of the nurses who has cared for him on a few of our days here is from Nigeria, and trained in London, Ontario at the University of Western Ontario. Katherine has been terrific, very responsive to our questions and concerns, and has allowed us to spend a lot of time touching Lukas and helping with little tasks like changing diapers. Dr. Dudell (the neonatologist) and the pediatric residents, particularly Dr. Cara Biddle, have been incredibly patient, explaining everything in detail, and making us feel as comfortable as possible.
11/26/2
Big day for our little guy today...after some initial uncertainty about when the surgery would happen, Lukas had his PDA ligated today. The surgery happened between 2 pm and 3 pm, which was probably the slowest hour Laura and I have ever experienced. Dr. Lee was the cardiovascular surgeon (looks a bit like James Earl Jones, the actor), assisted by Dr. Chen who was one of the pediatric surgery residents. They made a small incision under Lukas' left armpit, and then pushed the lung aside to expose the beating heart, aorta, and pulmonary artery. The aorta is the biggest blood vessel in the body, and carries blood to the rest of the body from the heart. The pulmonary artery carries blood from the right side of the heart to the lungs, where it can gain oxygen. The ductus arteriosus connected the two, and Dr. Lee said it was actually larger than the aorta. That is big, and means it definitely needed closing. They tied it off slowly, to minimize any changes in pressure that occur as the blood is shunted to its proper course, and then closed him up with tiny little sutures. They left a tiny little chest tube in place to drain any fluid that might collect after surgery, but this is just a routine precaution, and it should come out in a day or two. He is pretty sedated now, and will slowly awaken over the next day or so.
Lukas looks great - his color immediately improved from a dusky bluish color, especially in the lower half of his body, to a beautiful glowing pink color. Wonderful to see such a dramatic improvement in skin color so quickly after surgery. There is a bit of a recovery, but Dr. Dudell hopes that he will begin to require less support from the ventilator over the next day or two as a result of the corrected circulation.
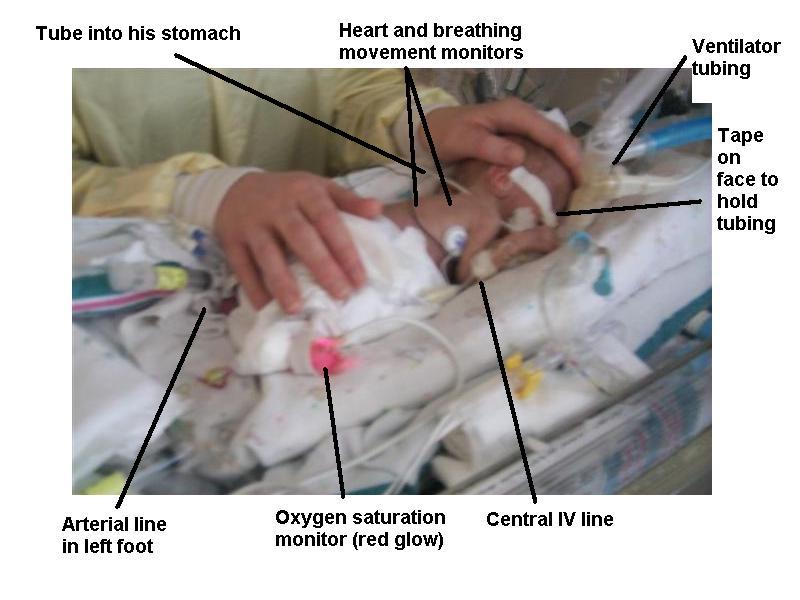
Our little guy has more lines than ever in him - two catheters in his veins, a catheter in the artery of his wrist, oxygen and heart monitors, the breathing tube, and now the chest tube. Whew. It will be good to see some of these disappear in the coming days, if all goes well.
11/27/2
Lukas was wrinkling his little forehead and making faces at us after lunch, and now we know why. Poop! Finally! One of our concerns has been that Lukas has not stooled. There could be a variety of causes, some not so serious (just a slow functioning gut, common in preemies) and some very serious (obstruction or rotation of the gut). A barium study has shown that stool was moving through the gut, and today we saw our first stool. That's the good news. The not so good news is that we were unable to switch Lukas over to the conventional ventilator today. He gave it the old college try, and spent about 90 minutes on the much quieter vent, but his carbon dioxide level went up and pH went down, so he had to go back on the high frequency oscillator. A chest x-ray showed that he had some atelectasis (basically, a collapse of airspaces in part of the lung due to lying on the right side after surgery on his left side) which was interfering with oxygen getting from the lungs into the bloodstream. They are doing some things to help break it up, so hopefully he'll be breathing easier tomorrow.
Our friends Allison and Gene visited today from Athens, and we went out for dinner after spending some time with Lukas. We hope that he makes progress over the weekend, and that the holiday doesn't slow things down too much. We're going to visit Athens for a few hours if all is well tomorrow. Thanks to all for your notes, but please don't be offended if I don't respond personally to each one. Some days it is all I can do to just upload this file, read a little, and crash. Happy Holidays, everyone, and raise a glass to Lukas when you are with your families.
11/28/2 (Thanksgiving)


Happy Thanksgiving everyone! We are certainly thankful for all of the love, support, and warm thoughts from our friends and family as we have all watched Lukas' progress over the past 13 days. We just had a great turkey dinner, prepared by Ken and Phyllis Bierema, with a fried turkey from Larry Hodge. Larry is a contractor in the Athens area who remodeled our house, and it was incredibly kind of him to bring us this very tasy turkey. It's also great for me and Laura to have a little time at home to do laundry, reload books and computer files, and see the dogs. Islay, our 10 week old golden retriever puppy, keeps getting bigger: go figure! Now Lukas just needs to do the same. Islay, in one of her rare calm moments, is shown at right. She is keeping Ken and Phyllis busy!
Lukas had a good day, with some reduction in his need for support from the ventilator, an indicator that the atelectasis is probably improving. We met the neonatologist who is on for the weekend, Dr. Augusto Sola, and he spent quite a bit of time explaining how Lukas was doing and what the plan is for the weekend. He is very hopeful that we are able to reduce his need for ventilatory support, and perhaps get him onto the conventional ventilator soon. So are we! We checked in with his nurse this afternoon just before dinner, and all was going well. We will be returning to Atlanta shortly (around 6 pm) and checking into our new hotel, one which has a fitness center. We're looking at one more week minimum of our November vacation in midtown Atlanta. ;-)
11/29/2
 When we returned from Thanksgiving yesterday afternoon, Lukas was requiring some dopamine to keep his blood pressure up. We spent some time talking to his nurse and the resident on call to try and figure out what had happened. As is often the case, there was probably more than one cause, and we may never know exactly what happened. Because his blood count was a bit low, we gave Lukas a small transfusion. It may also have been related to being started on phenobarbitol, a medicine being used to help him get rid of the bilirubin that has been building up, in combination with a slightly higher dose of morphine, the combination of which can cause blood pressure to drop. The good news is that during the morning today his blood pressure went up, and he is now off the dopamine completely.
When we returned from Thanksgiving yesterday afternoon, Lukas was requiring some dopamine to keep his blood pressure up. We spent some time talking to his nurse and the resident on call to try and figure out what had happened. As is often the case, there was probably more than one cause, and we may never know exactly what happened. Because his blood count was a bit low, we gave Lukas a small transfusion. It may also have been related to being started on phenobarbitol, a medicine being used to help him get rid of the bilirubin that has been building up, in combination with a slightly higher dose of morphine, the combination of which can cause blood pressure to drop. The good news is that during the morning today his blood pressure went up, and he is now off the dopamine completely.
Dr. Sola spent a lot of time with us today, which was much appreciated. We went over Lukas' cranial ultrasounds, which show some minor abnormalities, but he feels it is likely that they will improve on their own over time. There is no sign of serious or major brain problems, which is a big relief to us. Lukas' abdomen is still swollen, but felt a little softer today to the pediatric surgeon. There is a small collection of air in the region near his heart (pneumomediastinum) which is of little importance, and another small collection of air in the left lung related to the surgery (pneumothorax) which is more problematic. Dr. Sola spent quite a while positioning Lukas and working with his chest tube to try to get rid of that extra air. Part of the problem was that the tube was lying posteriorly, while the air was anterior. He put Lukas on his tummy, so the air would rise to meet the tube. So far, so good...his oxygen levels in the blood look good at this writing. We hope to try to put him on the conventional ventilator soon. This was a good day, and it is always easier to return to the hotel in the evening after one of those. Hopefully we can string together two or three in a row!
Allison visited today - it was great to see her, as usual. She and her husband Gene just finished a 13.2 mile race yesterday that finished about a mile from Grady Hospital. Way to go! We're hoping that Lukas will run that race in about 20 years. The picture at left shows Allison, Laura, and little Lukas lying on his tummy, showing us his better side. His head is in a stocking cap near Laura's left hand, and his bottom is in a white diaper.
11/30/2
Lukas had a quiet night, and was switched to the conventional ventilator today. After 12 hours, the blood gas measurements remain good, so we're cautiously optimistic. A blood gas takes a small amount of blood from the artery (arteries leave the heart and distribute oxygen rich blood to the rest of the body) and measures the levels of oxygen and carbon dioxide. Both are important - you want enough oxygen to supply the body's needs, and not too much carbon dioxide, a waste product that leaves your body when you exhale. He looks much, much more comfortable off the high-frequency ventilator, since his little body is no longer vibrating. I can't imagine what he has been through over the past 2 weeks - respiratory distress, heart surgery, a chest tube, numerous IV's and arterial lines, and constant vibration. Poor little guy.
Lukas' belly looks a little better today, slightly softer and a little pinker. He has been making a lot of urine, and the surgeon is optimistic that things will start moving soon. He required less morphine today for sedation after coming off the hi-fi ventilator (not surprisingly - spend two weeks on a blender and see how well you sleep afterwards!) We're hoping that they can take his chest tube tomorrow, assuming his chest x-ray looks good. The tube was placed to draw excess air out of the space around the lung, and appears to have done its job.
Laura's parents are on their way back to Michigan today. Max, Kudzu, and Islay have new dogsitters: Ken and Diane, Laura's brother and sister. They are taking a week's "vacation" in Athens, staying at our house, and helping out. It is incredibly nice of them, and we really, really appreciate it. Two good days in a row...hopefully tomorrow will make it three!
12/1/2002
When we arrived, the nurse had us wait in the hallway. Through the doors, we could see 5 people standing around Lukas, working intently. I guess three good days in a row was too much to hope for. Nothing terrible, but a bit of a setback this morning. The cardiothoracic surgeons stopped by and pulled out the chest tube. Unfortunately, they didn't first ask the neonatologists, who wanted to leave it in for a few more days due to the healing pneumothorax. Within minutes air started to reaccumulate in the space between the lung and pleura (the membrane covering the lung) and the neonatologists had to insert a new chest tube. This one is in a better position, and Lukas responded well. He probably lost a few hours of progress, though, and we hate for him to go through these procedures. Although the doctors numb the area and give pain medication, it is still no fun regardless of your size.
 The other issue is his digestive system. There is a tiny tube that goes through the nose and into the stomach. It has a little bit of suction on it, to suck up any fluid or bile. Overnight, that tube got plugged, and fluid built up in his stomach, duodenum, and small intestines. When they discovered the plugged tube this morning, they replaced it, and immediately got a large amount of greenish liquid out. That is good - it means that his liver is producing bile and that it is getting into the duodenum. The bad news is that it was unable to make it's way down the digestive tract and out into the stool. It appears that there is a plug or blockage of some kind near the end of the small intestine, just before the large intesting begins. There are a number of possibilities, including meconium (fetal stool) that has become thickened and formed a plug, barium from the upper GI study that has hardened, or both. The slow function of his bowel, with only very slow contractions of the muscle in the wall of the bowel, is probably contributing as well. We are going to put some little suppositories in his little rectum to try and get things moving a bit. If that doesn't work, they will do use an enema with some liquid contrast material (Gastrograffin) to try and loosen or dissolve the plug. If that doesn't work (remember, many if's here...) surgery may be required to remove the plug or even a small section of bowel if it has been damaged.
The other issue is his digestive system. There is a tiny tube that goes through the nose and into the stomach. It has a little bit of suction on it, to suck up any fluid or bile. Overnight, that tube got plugged, and fluid built up in his stomach, duodenum, and small intestines. When they discovered the plugged tube this morning, they replaced it, and immediately got a large amount of greenish liquid out. That is good - it means that his liver is producing bile and that it is getting into the duodenum. The bad news is that it was unable to make it's way down the digestive tract and out into the stool. It appears that there is a plug or blockage of some kind near the end of the small intestine, just before the large intesting begins. There are a number of possibilities, including meconium (fetal stool) that has become thickened and formed a plug, barium from the upper GI study that has hardened, or both. The slow function of his bowel, with only very slow contractions of the muscle in the wall of the bowel, is probably contributing as well. We are going to put some little suppositories in his little rectum to try and get things moving a bit. If that doesn't work, they will do use an enema with some liquid contrast material (Gastrograffin) to try and loosen or dissolve the plug. If that doesn't work (remember, many if's here...) surgery may be required to remove the plug or even a small section of bowel if it has been damaged.
 Dr. Sola, the neonatologist, Dr. Biddle, the pediatrics resident, and Dr. Gow, the pediatric surgeon all spent quite a bit of time with us today explaining what was happening. In my role as worried parent who happens to be a physician, I am especially appreciative of the outstanding communications skills that these physicians have displayed toward us. We are not easy parents to deal with, with more questions and an expectation for more detailed explanations than the average parent in the NICU. However, they have not been put off, and have actually seemed to enjoy the interactions with us. This we appreciate very much. A new team comes on board tomorrow, and we hope they are just as good at both the medical (tech) and personal (touch) skills of being a physician. We also appreciate the great care from the nurses and respiratory therapists - there is basically a nurse and an RT camped at Lukas' bedside round the clock, managing the minute-to-minute changes in blood pressure, oxygen saturation, pCO2 (carbon dioxide levels), and temperature. Very hard work, and it is so reassuring to us to know they are close by.
Dr. Sola, the neonatologist, Dr. Biddle, the pediatrics resident, and Dr. Gow, the pediatric surgeon all spent quite a bit of time with us today explaining what was happening. In my role as worried parent who happens to be a physician, I am especially appreciative of the outstanding communications skills that these physicians have displayed toward us. We are not easy parents to deal with, with more questions and an expectation for more detailed explanations than the average parent in the NICU. However, they have not been put off, and have actually seemed to enjoy the interactions with us. This we appreciate very much. A new team comes on board tomorrow, and we hope they are just as good at both the medical (tech) and personal (touch) skills of being a physician. We also appreciate the great care from the nurses and respiratory therapists - there is basically a nurse and an RT camped at Lukas' bedside round the clock, managing the minute-to-minute changes in blood pressure, oxygen saturation, pCO2 (carbon dioxide levels), and temperature. Very hard work, and it is so reassuring to us to know they are close by.
Finally, our friend Allison (see photo above), is a scientific illustrator, and made a pair of drawings to explain what a patent ductus arteriosus is, and how it is fixed. I love the Valentine heart (non-anatomically correct) attached to his little blood vessels!
Patent Ductus Arteriosus
PDA after ligation by the surgeons
12/2/2
Lukas had a quiet night, but was still requiring a fair bit of oxygen this morning. The x-ray helped us understand why - the atelectasis had returned in his right lung. With the air passages collapsed in part of the right lung, he only had about half of his lung available for oxygen exchange. The physicians made some changes in his position and ventilator settings to help reinflate the lung, and by the end of the day the FIO2 (percentage of air flowing into his lungs that was oxygen) was down to about 25% from 50%. That's good - a little progress in the right direction.
We also had progress at the other end, first a little "schmeer" of stool, then a nice healthy little bowel movement. We're so proud! ;-) This is also good news, since it suggests that his bowel may be starting to move a bit and that the obstruction maybe resolving. His bilirubin is also down further. All good. They are still following him closely, and we met the new surgeons (they change every week). Hopefully this means it is less likely that he will require some sort of surgery. He had another follow-up cranial (head) ultrasound, and the initial report was that it looked OK, but we're awaiting the official report. They also noticed that Lukas is hypothyroid - this means that the thyroid gland is underactive. In infants, this can lead to constipation, slow growth, and elevated bilirubin, all of which he has. If not treated within a month or two of birth, it can lead to brain damage, so we are happy that he got his first dose of medication today, within 2.5 weeks of his premature birth.
Laura got a visit from her colleagues Janet Truluck and Juanita Johnson-Bailey today, who whisked her away for a genuine Southern lunch at Marymac's, an Atlanta tradition. I saw patients this afternoon, and it was good to see our staff at the office and do something productive for a change! I also stopped by our house to say hello to Ken and Diane, who are housesitting and will be visiting us tomorrow. His new neonatologist is Dr. Theresa Gauthier (gowtee-ay), and she's terrific. Very down-to-earth, she communicates well with us, is very experienced, and is obviously very up-to-date. Being a good physician means knowing the best evidence, and then having the wisdom and experience to apply it appropriately to the patient in front of you. She has these skills.
12/3/2
Today was less encouraging. Lukas's heart and lung function was stable, but his belly was more distended this morning. He got a couple of enemas today, one with warm saline (salt water) and one with Mucomyst, to help get things going. The latter helps break down sticky fluid, and resulted in a small BM later in the day. However, we suspect that this won't be enough, and that he will require a further enema with gastrograffin (a contrast material) under fluoroscopy. Fluoroscopy is where you get a "moving x-ray image", so the doctor's can carefully monitor the injection of contrast to avoid damaging his tiny and delicate bowels. This will probably occur later tomorrow; the radiologist comes to Grady from Eggleston Hospital, we are told. Because they can monitor things under fluoro, they can be a bit more aggressive and hopefully have a better chance of clearing any obstruction. If not successful, I suspect our little guy will have surgery to follow, perhaps later tomorrow or Thursday.
Lukas also had an increase in bands in his blood count. These are immature forms of white blood cells. While it could just be his bone marrow starting to crank up, it could also indicate infection. He has been off the most powerful antibiotics on the planet for a whole 48 hours now, so I guess it's time to go back on, eh? His bilirubin also edged up again today, which could be a sign of infection. Likely sources of infection are his lines (IV, arterial, chest tube) so those were cultured. If cultures don't grow anything and he looks OK after 2 days, they'll stop the antibiotics again.
Ken and Diane visited today, brought some goodies (OK, everyone, we officially have enough snack food now!), and Diane cut Laura's hair. We lunched on Thai food in Virginia Highland - beautiful day today, sunny and 60's. We are now at 5 Thai restaurants, and each has been excellent.
12/4/2
Last night I dreamt that Lukas had hydrocephalus (enlarged ventricules with fluid in them in the brain, that can lead to brain damage). He doesn't, but I had to keep reminding myself every time I worke uup that his cranial ultrasound was normal. I asked Dr. Gauthier, the neonatologist, about the official reading on his cranial ultrasound of 2 days ago, and it was read as normal. That is great - the minior changes seen at Days 1 and 4 appear to have resolved.
I returned to the bedside after a short break, and found that he was breathing at a rate of 100 breaths per minute. While the ventilator was going at 45 bpm, he was adding another 55. Try breathing at a rate of three times every two seconds for a while and you'll see how it feels. This high rate was new, and it was clear that something was bothering.him. I called for his physician, who found that the site of the first chest tube was leaking greenish fluid. This is probably green because of bil tinging it, but it could also be a sign of infection. The thoracic surgeons put a suture in to close the leak, hopefully taking care of that problem.
Lukas went down to the radiology department today. This is quite a production - he was switched to a new ventilator, put in the same sort of portable incubator that he had been on coming from Athens, and took the elevator down accompanied by a large entourage. He tolerated the study very well, with no loss of oxygen levels (desaturation) despite being put on a table out of the incubator, lying on his belly and side, and lots of manipulation. He's a tough little guy, my son is. He is now back upstairs and doing fine, although his belly is still big. As it turns out, the obstruction appears to be in the terminal ilium, which is the last part of the small bowel, just before the colon. The colon looks OK, and had a little meconium in it. The bad news is that he will require surgery to correct this, probably tomorrow. Two major surgeries in his first 3 weeks of life, before ever weighing 2 pounds. That's a lot to bear. Think good thoughts, everyone.
12/5/2
Lukas is in surgery as I write these words. We met the surgeon, Dr. Barbara Pettit, who is Chief of Pediatric Surgery here at Grady. We were very impressed with her, both her confidence and her skill in explaining what she thinks is probably happening. Laura and I are waiting now - it should take about an hour. Lukas is doing OK otherwise, but the surgeon warned us that he is almost certainly going to look and do worse over the next two or three days before he starts getting better. This is terrifying, there is no other way to put it. Laura and I have both been nauseated all morning out of fear.
Auguste Rodin, the sculptor who created "The Thinker", said: "Patience is also a form of action." After over 2 hours of waiting, when the surgery was supposed to take only an hour, we have to remember that. They finally brought our Lukas back after 2 1/2 hours. He did well, and his little belly is much smaller. Here is what happened:
1. They make a large (for him) incision across the abdomen, below the bellybutton.
2. They inspected his intestines, and found that there was an area of narrowing (stenosis) near the end of the jejunum. The small intestines consist of the duodenum, then jejunum, and then ilium. Beyond that stenosis, the ilium was very small, as was the colon. That is probably because they were never really used, since use causes them to stretch to normal size.
3. They removed the stenotic section of small intestine (a very short length) and sent it to the pathologist for examination. One possibility, although relatively unlikely, is that Lukas has Hirschsprung's Disease, a congenital lack of nerves in the colon. This would require further surgical correction, but kids generally do pretty well afterwards, just have 3 or 4 BMs instead of 1 or 2 per day.
4. They also found a plug of meconium, and then a large plug of barium and stool. These were removed through the opening in the bowel made by the surgeon. One concern has been that Lukas has cystic fibrosis, since that can cause these meconium plugs. The surgeon and neonatologist think this is unlikely, but tests are pending.
5. The surgeon took the two open ends of bowel and attached them to the abdominal wall, creating two small stomas (openings) in the skin (see diagram at below). He will stool through the one that empties his proximal bowel; the other is connected to the distal segment of bowel. (Proximal means closer to the beginning of a structure, in this case closer to the mouth, and distal means further from the beginning) The good news is that they can start using his bowel pretty quickly, hopefully within a few days. Then, when he weights 4 1/2 pounds, they will reconnect the ends of bowel assuming that he doesn't have Hirschsprung's.
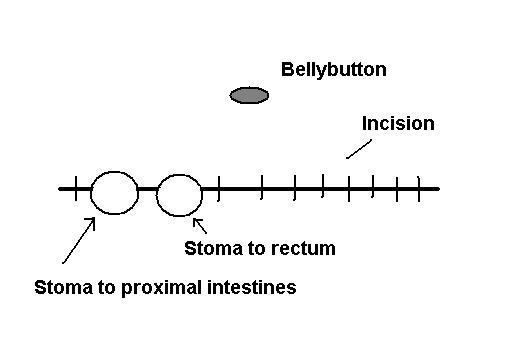
6. His liver looked a little inflamed and nodular. This is probably just because he has been sick and has not been able to use the bowel, being sustained instead by nutrients in an IV. This will hopefully improve over time and progress to full recovery of liver function.
7. The incision was closed; the stomas are in the suture line. The incision was covered with gauze and his belly was wrapped with stretchy gauze to keep it in place (no tape). There is a handwritten note on the dressing that says "Good luck Lukas!". ;-)
Dr. Pettit and the intern, Dr. Andrew Bullock (of Athens!) did a great job of walking us through the surgery and explaining what had happened. They were gracious enough to pose for a photo, despite having just spent nearly three hours in an operating room kept at 88 degrees fahrenheit to keep our boy Lukas comfy.
It is going to be a rough few days for our son Lukas. We are very hopeful that he doesn't have any serious underlying problem like CF or Hirschsprung's - it's bad enough to have been born too early and too small. Fortunately, there is no known association between CF or Hirschsprung's and IUGR or oligohydramnios, his two original problems. The latter were probably related to a placental problem. That in turn could have led to a lack of blood flow to part of the bowel, leading to the stenosis, leading to the obstruction, and then leading to the liver problems. I'm a big believer in Occam's Razor, as are Lukas' doctors, which is why we think two rare things at once (i.e. CF plus IUGR/oligohydramnios) is so unlikely. Occam was a Greek philolsopher who said that given two possible explanations, the simplest is the most likely to be correct. Lukas having CF or Hirschsprung's on top of IUGR and oligohydramnios and placental insufficiency would be like lightning striking twice in the same spot on successive days. It can happen, but it is incredibly unlikely, since these illnesses are not more common in kids with IUGR.
 So...keep thinking those good thoughts, keep your fingers and toes crossed, and wish Lukas well as he works on recovering. Key goals over the next few days will include improvement in liver function, ability to use his gut, stabilization of his fluid requirements, improvement in blood pressure and heart rate, reduction in ventilator settings, and avoidance of infection. Long list for a little guy.
So...keep thinking those good thoughts, keep your fingers and toes crossed, and wish Lukas well as he works on recovering. Key goals over the next few days will include improvement in liver function, ability to use his gut, stabilization of his fluid requirements, improvement in blood pressure and heart rate, reduction in ventilator settings, and avoidance of infection. Long list for a little guy.
12/6/2
Lukas had a rough night, and kept his nurse Kelly busy trying to keep his blood pressure up, heart rate down, and oxygen saturation in a healthy range. When we came in this morning, his mean arterial pressure was only about 26 or 27; it should be in the 30's for his size. Keeping it even that high was requiring 18 mcg/kg/minute ("18 mikes") of dopamine. Dopamine is a pressor, so named because it keeps blood pressure up. However, it can do bad things, and ithe less of it the better. Fortunately, by this afternoon (as I write this entry) his blood pressure is running closer to 35, and he is down to only 10 mcg/kg/minute of dopamine. Good day so far for Lukas! He also got his chest tube out, properly this time, and tolerated the procedure well. Since he was peeing around his catheter (i.e. urine was leaking out around it) that tube was removed as well. All good - it's nice to see more Lukas and less tubes as time goes by. He still has the ventilator tube, arterial line, central IV line, oxygen sensor, heart sensors, and a peripheral IV. But progress is progress.
Diane and Kenny, Laura's brother and sister, stopped by again to visit. We discovered a fantastic Cuban/Spanish restaurant called La Fonda Latina - a big helping of paella for $8 made Mark a happy boy at lunchtime. Our friend George will have to go there next time he is in Atlanta.
Allison is at it again...below are some sketches that further illustrate Lukas' surgery and planned recovery to normal bowel function. Thanks, Allison! He's becoming our illustrated little man.

Lukas is getting terrific care from his nurses here at the Grady NICU. While I have worked with nurses for many years, in a way we operate in parallel universes. With our hospitalized patients, we physicians swoop in once or twice a day, write some order, and leave. The nurses provide the care and manage the myriad hour by hour and minute by minute changes in the patient's condition, and make sure that what needs to happen. All too often us medicos do not properly appreciate the nurse's contribution or level of skill. Boy, are we wrong. Sitting here for 12 hours a day, I have received an education in NICU nursing, and am incredibly impressed by what I see them do for Lukas. At left are his nurses for today, Marie and Danali...thanks, guys!
12/7/2
We received a phone call at about 8 AM this morning at our hotel that caused us a moment of terror - as far as we knew, the only ones that have this number are the nurses at the hospital, so they can call us if there is something wrong with Lukas. Fortunately, it was someone else, and Lukas was fine. The best way to reach us is with email, since every time the phone rings these days we panic. Plus, we just don’t have the energy to take a lot of calls. Despite our limited internet access, we generally respond to emails within 24 hours. We truly appreciate every good thought and gesture, and hope you will understand our request.
Lukas continues to recover well after surgery. He was down to 6 'mikes' on the dopamine, and lower settings on the respirator. His labs were OK, and he was starting to get green stuff out of the stoma, which is what you want it to do. The goal over the next day or two is to get him off the dopamine. Then, we can start to give him small amounts of breast milk. Over the next week or so we will be looking for him to continue to require less support from the ventilator (a process called 'weaning'), see his bilirubin go down, see him successfully use his gut with small amounts of breast milk, and avoid infection. We also have some important test results pending, so I'm sure it will be a busy week for everyone. Beyond that, we hope to see him get off the ventilator in 2 to 3 weeks, and get back to Athens by Christmas. Of course, that means the Athens NICU, not our home. The best we can hope for is getting Lukas home sometime in the first quarter of 2003. And of course, all of these 'ifs' depend on continued progress and no major setbacks.
Laura and I took advantage of the good day to dash back to Athens for laundry and reminding our dogs who we are. Islay is growing quickly, and is now (pretty much) housetrained, thanks to the Bierema family. Laura's brother Ken is doing some projects around the house, which we appreciate very much. The garden shed that we started building a couple of months ago is now done, and the next step is to renovate the garage into a guest room/play room/exercise room.
12/8/2
Lukas had a quiet night, maintaining his blood pressure and oxygenation, and putting lots of liquid out through his stoma. His tummy was more swollen yesterday afternoon, which is expected after surgery. This is called 3rd spacing (the first two spaces are intracellular, i.e. fluid in cells, and intravascular, i.e. fluid in blood vessels) and happens post-operatively for a variety of reasons. If anything, he had somewhat less than expected, and should get rid of this fluid over the next few days.
Our little guy was quite active this morning, opening his eyes and looking at us, responding to our voice (or at least appearing to), wrinkling his brow in annoyance when he was being weighed, and moving his arms and legs. They are decreasing the amount of morphine, since too much morphine suppresses his drive to breathe and also lowers his blood pressure. The result was good - he is now completely off the dopamine that was being used to keep his blood pressure up, and his last blood gas was quite good. The blood gas measures pH (acidity/alkalinity), carbon dioxide (CO2) level, oxygen (O2) level, and bicarbonate. Good blood gasses allow us to turn down his ventilator settings a bit, then check another gas in an hour or so to see how he tolerated it. If the follow-up blood gas is good, then these become his new settings till the next attempt at weaning. It is a slow process, but remember, patience is also a form of action.
12/9/2
 Lukas had another quiet night, and a good day. They are manipulating the ventilator settings in an effort to get him to do more of the effort of breathing. Basically, when he makes an effort, the ventilator kicks in and delivers a good sized breath. If he poops out, there is a "back-up" setting to make sure he gets enough breaths. He has been relying on the ventilator to breathe for him, so he has to build up those chest wall muscles and exercise his diaphragm so he can do the work of breathing without needing a ventilator. This will take time - sort of like training for a marathon, as Dr. Gauthier puts it.
Lukas had another quiet night, and a good day. They are manipulating the ventilator settings in an effort to get him to do more of the effort of breathing. Basically, when he makes an effort, the ventilator kicks in and delivers a good sized breath. If he poops out, there is a "back-up" setting to make sure he gets enough breaths. He has been relying on the ventilator to breathe for him, so he has to build up those chest wall muscles and exercise his diaphragm so he can do the work of breathing without needing a ventilator. This will take time - sort of like training for a marathon, as Dr. Gauthier puts it.
The surgeon stopped by - Dr. Ricketts took over for Dr. Pettit today. He was pleased with his progress, and we are hoping to see him use that newly unobstructed gut soon. Labs looked good today too, especially the bilirubin which dropped to its lowest level ever of 4.4 total and about 3 direct. It had been as high as 15, with a direct bilirubin of over 10, just a week ago. Hopefully this is good news for his little liver. Other tests are still pending.
He is still a tiny little boy...while his weight is about 900 grams now, it is unclear how much is Lukas and how much is extra fluid. He is definitely more active, waving his arms and opening his beautiful blue eyes to look around. Below are some photos of Lukas, including a close-up, and a picture of one of his favorite nurses, Katherine (see 11/25/2 note above). What a heartbreaker! Another one of his nurses, Monika, called in on her day off to see how he was doing. We appreciate her thoughtfulness.
 Many people ask how we are holding up. Laura and I are doing quite well, actually. While we both knew deep down inside that we married the right person, it is nice to have it confirmed under these trying circumstances. We are also deeply appreciative of all the people that have sacrificed and pitched in to help us be here at Lukas' bedside, especially our parents Ken and Phyllis Bierema and Herbert and Hildegard Ebell; Laura's brother and sister Ken and Diane; the faculty and staff at the University of Georgia's Department of Adult Education who have covered much of Laura's work; and the staff at my clinic who have helped me not feel guilty about missing afternoons of patient care.
Many people ask how we are holding up. Laura and I are doing quite well, actually. While we both knew deep down inside that we married the right person, it is nice to have it confirmed under these trying circumstances. We are also deeply appreciative of all the people that have sacrificed and pitched in to help us be here at Lukas' bedside, especially our parents Ken and Phyllis Bierema and Herbert and Hildegard Ebell; Laura's brother and sister Ken and Diane; the faculty and staff at the University of Georgia's Department of Adult Education who have covered much of Laura's work; and the staff at my clinic who have helped me not feel guilty about missing afternoons of patient care.
12/10/2
One of the earliest concerns raised by the neonatologist in Athens was that Lukas may have a chromosomal abnormality of some kind. Most commonly, this involves a missing part of a chromosome, an extra chromosome ("trisomy"), or a translocation where some material from one chromosome ends up in the wrong place. This was a concern because chromosomal defects are a fairly common cause of severe IUGR, and also because his eyes were very slightly downsloping initially, and his ears were a tad low. These abnormalities are a common feature in dozens of chromosomal problems. The first couple of attempts to grow his cells in the lab (a necessary part of chromosomal analysis) failed, but fortunately the third time was the charm. Best of all, Lukas is swimming in the deep end of the genetic pool - he is a normal, healthy, boring, XY chromosomally normal little boy. Whew! This has been hanging over our heads for 4 weeks, and it is an amazing relief to hear this. Other tests for CF and Hirschsprung's are still pending, but it's great to get this one back as normal.
As Lukas has gotten older (he'll be 4 weeks on Thursday) his face has filled out a little bit, making his eyes less slanted and his ears a bit higher. We're both confident that he will be a particularly good looking little boy - as long as he got Laura's looks. He certainly got my temperamant!
We are making some progress weaning today, with the volume of air pushed into his lungs decreased from 4 ml to 3 ml over the past 24 hours. To give you an idea, a teaspoon is 5 ml. The rate is down from 55 to 50 over the past 3 days, and the percent oxygen going in is hovering between 25% and 32%, depending on how he is feeling (room air is 21% oxygen). The physical therapist spent quite a bit of time with us and Lukas today, instructing his team how to position him to protect his little hips. Babies in the uterus are cuddled up in the well known fetal position, but in the NICU Lukas has spent a lot of time splayed out like a frog on the dissecting table (sorry for the analogy, but you get the idea). While we have been moving him from side to side, it is still quite different from his position in utero. To assist in this process, I ordered a few batches of teeny-tiny little diapers, each about the size of a sanitary napkin. Grady doesn't stock ones this small, and the concern is that the larger diapers are pushing his hips out of position, which could lead to problems down the road.
In a related effort to keep him good-looking, I also ordered some little gel-filled pillows. They will cushion his head, and prevent the "flathead preemie" syndrome that can happen in these tiny ones. He has spent much of today on his tummy, with his head turned to the side, as a way to help his breathing even more. Good to see another side of our son today. He is tolerating it very well - I have been watching him work hard, getting his oxygen saturation up above 95%, then poop out a bit, his oxygen saturation dropping below 85%, which triggers an automatic reflex to get him to work harder on his breathing. As my track coach Mr. McCauley used to say, "No pain, no gain", and "The only place that success comes before work is in the dictionary". This applies to Lukas breathing training regimen, I think.
12/11/2
Today was quiet. While this is good (nothing bad happened) it is also frustrating, as there was essentially no action on the intestinal front. To give the little guy some credit, he did come down a bit on his ventilator settings, from 50 to 45 breaths per minute of back-up rate, and from 3 to 2.7 ml tidal volume. That's definitely the right direction. If it wasn't for his still swollen tummy, he'd be getting close to coming off the ventilator. That's because his big tummy is pushing up against his chest, and increasing the work it takes to expand his little chest.
Regarding his tummy, we are still waiting for his bowel to start moving. Preemie bowels are notoriously finicky, often taking quite a while to start moving in the right direction, and especially when the intestines were subjected to surgery. Part of the surgery involved pulling his intestines out of his body and "running them", i.e. squeezing them to get the collected stool and barium out. This is very traumatic, and it isn't unusual (apparently) for it to take one or even two weeks for things to start moving. Very frustrating. Plus, as I write this it is 5:45 pm, and the surgeon hasn't been by yet. I suspect they may not come by at all today, which is annoying. The neonatologists have seen and examined Lukas several times, so he is getting attention, but it would be nice to have the surgeon stop by.
We had some sad news yesterday. Laura's aunt Sharon (her father's younger sister) died suddenly yesterday morning. Sharon was a very sweet and thoughtful woman, and our hearts go out to her husband Bob and daughter Cynthia as they struggle with their unexpected loss. Her death was totally unexpected, which makes it even more difficult for everyone.
Laura's father Ken, who was driving down to Georgia to take over on dogsitting duty, had to turn around halfway through Indiana, and her brother is on his way back to Michigan for the funeral and a wedding. Our friends Allison and Gene have graciously "adopted" our puppy Islay for the time being, and our housesitter Tanya is watching Max and Kudzu, our older goldens. We hope to (maybe, fingers crossed) spend Saturday evening in Athens. We'll see how things go.
One other good thing - my quest is over. After searching about 15 Thai restaurants nationwide, including 6 here in Atlanta in the past 3 weeks, I have finally found the perfect Thai fried rice. My alltime favorite is that dish (Kao Pad Prik, chicken, medium up hot on their menu) at Siam Spicy in Detroit, where I ate weekly (at least) for 4 years. Now, finally, a dish just as good. King and I Thai Restaurant, on Peachtree near Monroe, at the back of a little strip mall. Now I just have to convince Laura to eat there every night. ;-)
12/12/2
Below is a picture of Lukas with his various wires and tubes labeled...as you can see, he is pretty well tied down. While he moves his arms and hands back and forth and looks around at us, he of course can't roll over or lift his head yet, and relies on his nurses to position him. Below, he is lying on his tummy; those are his mother's hands comforting him. Preemies seem to like gentle, firm pressure rather than stroking or rubbing. I apologize for the blur, but the room lights are dim and we don't want to use a flash that might harm his eyes. The incubator is open now - it is a cylinder, and the top half rotates around to expose our little guy. There is a warming lamp above, especially helpful when the incubator is open. When closed, a formfitting blanket is draped over it to provide protection from light and some additional sound protection.
Today was fairly quiet, after a rough start. Because we were in the noisiest part of the unit, and the administration is apparently incapable of enforcing any rules about keeping the area quiet, our son had to move to a different and quieter section across the hall. This is a bit of an ordeal, with a respiratory therapist and two nurses working on him the whole way, using a bag to help him breathe while the ventilator was unplugged. You think they would invent a battery pack that could last 5 minutes for the transfer. Anyway, after a few hours of requiring higher oxygen levels, he was back down to room air or a little bit over room air by the early afternoon. He also pulled his "Anderson," a thin tube in his stomach, out of his mouth. Tired of it, I guess. Feisty - that's my son! It will be replaced with a smaller tube that is more comfortable, and hopefully this will be adequate to drain any fluid that builds up in his stomach. Not much came out of the old tube today, which is good. Hopefully his digestive juices are starting to move in the right direction. He also blew a little gas out into the stoma bag - no father was ever happier that his kid farted in public. ;-)
This evening, they dropped his rate on the ventilator from 45 to 40, which is good. I thought that might be a bit much, and sure enough his CO2 rose a tad, and they had to back off a bit and set the rate at 43. This is still better than he started, so he continues to make progress.
12/13/2
Today is Friday the 13th, and it has been an up and down day. The surgeon and neonatologist are both increasingly concerned that Lukas is losing protein out of his gut and into the ostomy bag, instead of hanging onto it like he's supposed to. His protein level in the blood is very low, leading to the swelling in his abdominal cavity and elsewhere, which is in turn making everything else worse. The pediatric pathologist from Emory University looked at the sections of tissue from Lukas' small bowel, and said it looked normal except for some edema (swelling, usually caused by inflammation). He saw normal nerve ganglia, meaning that Lukas doesn't appear to have Hirschsprung Disease, and he said the mucosa (lining) does not look like that seen with cystic fibrosis. So far so good - those two diseases appear very unlikely now. Apparently the neonatologist was more concerned that we had thought about CF, and she was visibly relieved.
However, it doesn't explain why Lukas continues to lose protein through his gut, which is known as a "protein-wasting enteropathy". These can be caused by changes at the molecular level in how the gut moves chemicals into and out of the bloodstream, and the gut lining may even look normal under the microscope. Sometimes this kind of enteropathy can occur after surgery, particularly in kids who are premature and sick (like Lukas). However, it can sometimes be a sign of a very serious inborn problem with how the gut functions. While Lukas' small bowel is showing signs of moving in the right direction, that mechanical function moving food and waste in the right direction is only part of the gut's function. The more critical part is absorbing nutrients from food and excreting waste products into the stool, and this isn't functioning properly, since he is pouring protein out into the stool. We hope that it is something that will correct itself, and should know more over the next few days.
Dr. Gauthier spent quite a bit of time today following up on Lukas' test results, and helping us understand them. She gave each of us a hug, and we know that she is doing her best to help Lukas do just as well as he possibly can.
12/14/2
Lukas had a quiet night, and his ventilator settings continue to improve. His gut is working in a mechanical sense (moving gas and liquid in the right direction), but is still pouring out watery (serous) fluid. Our hope is that he will eventually start putting out something that looks a bit more well-formed - not exactly stool, but not runny clear liquid either. As the attending physician today said (it is Dr. Cornish, "like Cornish hen", he told us), Lukas has the world's worst case of diarrhea. Until that resolves, we can't use his gut to give him nutrition. They are increasing the protein and lipids in his intravenous fluids, with the hope that the protein and lipids stay in the blood vessels, and in doing so draw the extra water out of his gut, into the blood vessel, and out through the kidneys. If his urine output goes up over the next couple of days, we'll know it's working. If, on the other hand, his blood vessels are leaking protein, then the ascites (fluid in the abdominal cavity) and urine output will not improve, or might even get worse. It is (yet another) waiting game, with Lukas calling the shots. Dr. Cornish spent quite a bit of time talking to us, which was much appreciated.
We are going to spend tonight at home, and return in the morning. It will give us time to do laundry, and attend a couple of Christmas parties that are scheduled for this evening. The attending physician today said that he had seen a couple of cases that were in some ways similar to Lukas where it took months for the gut to recover, but once it did, the kids were fine. It is hard to fathom being here for months, but if we have to, we have to. Laura and I have done a lot of bike touring on our own, just packing up the bikes and panniers, flying to a country, buying some maps, and riding. We've done it in the US, Canada, England, Ireland, Scotland, Netherlands, Belgium, and Germany. During those tours, some lasting up to 5 weeks, we have come up with a variety of "lessons learned". They include:
- Balance is important
- Rain stops
- It is what it is, and we'll ride over it
- Keep your mouth shut
- Pack light
- Keep lines of communication open
- There will be good days and bad days

Today, I'll talk about the first lesson: Balance is important. In 1995, we flew to Shannon, Ireland, and after a long night on the plane, and a couple of hours putting the bikes together, attaching the racks, and strapping on the panniers (saddlebags) we were finally ready to go. We wobbled off, and immediately got lost. Laura's bags weren't well balanced, and while making a tight U-turn in a subdivision near the airport, Laura tipped over. She broke the rear-view mirror, scraped her hands, and bruised her ego. We spent a little while shifting her gear around, and with a better balanced load, she never fell again. Balance is important in life, too, and during this time we have tried to spend a little time each day exercising, reading, eating a good meal, and drinking a glass of wine. It is hard not to feel guilty, enjoying something while Lukas suffers, but we have to remind ourselves that flagellating ourselves won't make him suffer any less. Balance is important, and we will continue to seek it.
Tomorrow, I'll talk about the next lesson. Until then, look at this nice clear, sharp photo of our son Lukas. His eyes were closed, so I felt comfortable using the flash. There is quite a bit of swelling around his eyelids (caused by the low protein) but his eyes are a beautiful blue when open. He even smiled a bit for us yesterday, which is hard for us to imagine, given his situation. His fingers are long and graceful and very beautiful.
12/15/2
We had a very nice trip back to Athens. Our friends Phil and Carolyn Holmes had a lovely Christmas party, and we had a chance to see some good friends. Later in the evening we joined Laura's faculty for their Holiday party, which included a white elephant gift exchange. I actually got something I wanted - a book by John Feinstein called "A Good Walk Spoiled", about life on the PGA tour. Sometimes one man's trash is another man's treasure. After a quiet morning with some good coffee in real mugs and the NY Times (both of which we love but have largely had to do without), we drove back to Atlanta and Grady Hospital.
It was good to see Lukas again, but also hard to see him; his little tummy is still incredibly swollen, and is totally out of proportion to his very delicate head, chest, arms, and legs. His scrotum is somewhere between the size of a golf ball and tennis ball, which is of course hugely swollen for him. It is swollen because there is a direct connection between the abdominal cavity to the scrotum, through which the testicles descend during development. This is called a hydrocele, and in his case, with the ascites (extra fluid in the abdominal cavity) it is the mother of all hydroceles. We have a hard time looking when they remove the diaper. Yesterday they began giving Lukas some albumin, and it appears to be staying inside the blood vessels, which is good. His serum albumin level went from 1.8 to 2.7, which is quite a jump. His urine output is also good, which we hope will eventually help get fluid out of the abdominal cavity. However, he is still pouring a large amount of fluid out into his ostomy bag. There was a little blood in the ostomy output last night, but that appears to have stopped. So, for now we hope that his ostomy output slows and becomes more formed, that his urine output increases, and that his abdomen and scrotum become less swollen. At best, this will take days, at worst weeks or never.
Lesson #2 from our bike tours was: Rain stops. Our longest tour was 5 weeks through Ireland, Scotland, Belgium, and the Netherlands, and was a wet affair. Every single photo taken of us on that tour shows us in our yellow GoreTex rain gear, usually uppers and lowers. But one thing we kept reminding ourselves during this trip was that rain does eventually stop, even if it takes longer than you'd like. There is a similar but much more cynical aphorism in medicine, that all bleeding stops. Unfortunately, it sometimes stops because the patient dies. But it does stop. We want the very best for our son Lukas, and want the fluid accumulation to stop, the protein loss to stop, the lung injury to stop, and his suffering to stop. We know it will, but also realize that it may not stop in a way that leaves him with us. Over the next few weeks, we will try to remember that this won't go on forever, and that for now we have to do everything we can to make him feel loved, and feel as comfortable as possible while he tries to recover.
12/16/2
When we arrived this morning, we ran into the resident Dr. Schaeffer in the hall. She said that Lukas had had a rough night. We had noticed yesterday that he was less interactive, especially in the afternoon. Antibiotics had been stopped about 24 hours before, and it looks like that lassitude was the beginning of sepsis (severe infection and the body's response to it). His little tummy was very red, and the stoma site was breaking down, with skin separating from the bowel mucosa where it joined the skin. The ostomy nurse spent quite a bit of time dressing the wound, and he is now on three antibiotics again (vancomycin, amikacin, and clindamycin).
The new surgeon, Dr. Parker (they change weekly) felt that the protein loss and other problems could primarily be caused by the liver, and that as his liver improves, these other problems and the wound healing will as well. Lukas' stoma output has decreased, which is encouraging, so he isn't losing as much protein, and his bilirubin is down to 3.7 total, 1.3 direct (best ever). His tummy even looks a little better in terms of its size. However, he is requiring higher ventilator settings (33% oxygen, rate of 60, up from 40). Lukas is acidotic from the sepsis, and the body gets rid of extra acid by turning it into carbon dioxide and breathing it out.
His little face and hands and arms are puffier. In a way, this makes him look more "normal", like a chubby cheeked little baby. Kids with IUGR typically have little baby fat, and look like wizened old men. The edema has filled him out, and we can get a better idea of what our son will look like when he gets older and fills out. We both agree he will be incredibly handsome! We had a really nice 30 minutes, with him holding our fingers and smiling and eyeing us. Yes, smiling, if you can believe that. What an incredibly brave little guy.
Lesson #3: Is is what it is, and we'll ride over it. Laura and I were riding our bikes on Vancouver Island, and staying at the wonderful Yellowpoint Lodge. The primary exercise at the lodge was walking from our adirondack chair on the water to and from meals. While sitting there, looking across the water toward Saltspring Island, I mentally traced our next day's route. Looking at the map, and the island, I saw that we had a huge hill to climb. I began to worry that we wouldn't make it to Victoria, our destination the next day, because it was about 90 miles, and with hills like that, well, it would be a long day. However, worrying about it wasn't going to make the hill any smaller, and we were good riders with good equipment who had ridden further in a day and ridden up higher hills. After a while, we both agreed: it is what it is, and we'll ride over it. That has become a mantra for us whenever faced with a tough situation, and we have said it from the first day. We think Lukas will be a great biker some day, and have long dreamed of taking him with us when we are touring in Germany or the Netherlands or northern Michigan. We think he knows that he's strong, he has great medical care, and parents that love him: it is what it is, and he'll ride over it.
12/17/2
Lukas had a somewhat better day today. His white blood count and platelets were up a bit (this is good - they had been low, which happens with sepsis in preemies), his belly and scrotum are no bigger (maybe even a bit smaller), and ventilator settings are improved. They were able to reduce the tidal volume, which is the amount of air going into his lungs, from 5 ml to 4.5 ml, and the rate from 60 to 55. Best of all, he just plain looked better. Better color, and some good interactions when the morphine was wearing off and he woke up. It was otherwise a quiet day, with no further testing, and we hope that Lukas took advantage of the rest to get stronger, and continue to fight the infection.
Lukas got a new tube that goes from the ventilator into his lungs. It is a bit larger - the old one was too small, and some of the air being pumped in was leaking out. Take a soda straw, purse your lips around it, pinch your nose, and try to breathe through it. That's what Lukas is doing, so he appreciates the bigger tube.
Here is a photo of our new office - note the attractive view of the hospital parking lot, the expansive workspace, comfortable seating, and excellent lighting. It actually isn't bad, and we both get a fair bit of work done between chances to look at Lukas. Note the laptop on the little 1 x 3 foot table, and colored folders with Laura's student's papers. The incubator is usually completely covered to give him a dark, quiet environment in which to rest.

Lesson 4: Keep your mouth shut. When biking in the countryside, you often ride alongside ponds, ditches, streams, and rivers. These are great breeding places for bugs, and those bugs have a way of finding their way into your mouth when you ride. Considering that my mouth isn't that big (maybe 1-2 square inches in casual openness) it's amazing that you can get 20 or 30 bugs a minute in there during a bad stretch! Therefore, on stretches like that, on days when the air is buggy, we learned to keep our mouths shut. As a physician with a critically ill child, I've also had to learn to keep my mouth shut, with varying degrees of success. While Laura says I'm doing really well, I suspect that she's being kind. Most days there are at least a few times where I make "helpful suggestions" to the nurses and physicians. The attending on call over the weekend sat me down and gave me some "friendly advice" to not talk to anyone except the attending, and then only once a day. He had asked if I had any questions during rounds, and when I actually did, and also made some suggestions, I think he was a bit taken aback. While his advice was well intentioned, and may have worked for him when he had an ill child, I don't have such an easy time turning my brain or mouth (which are closely connected...sometimes too closely) off. So, I will continue to make the occasional suggestion, will try to limit most of my interactions to a chat with the attending, and will make sure that I am respectful and thankful for the terrific care that Lukas is getting from his healthcare team.
12/18/2
Another relatively stable day. Lukas had a bigger belly this morning, but his color was good, and surgical sites and stoma looked good to the surgeon. He was wondering out loud if maybe all of the fluid leaking into the ostomy bag was perhaps leaking from the belly around the stoma, rather than coming from the gut out of the stoma. They will be doing an ultrasound to look at the liver - perhaps some venous obstruction in the liver is causing the fluid collection in the peritoneum. We'll see the results tomorrow. Lukas' labs and ventilator settings were stable today, and we had a really nice interaction in the evening. He seems most comfortable and interactive in the early evening, when things quiet down in the NICU. His facial expressions make it very clear when he is in pain - play with an IV or poke him, and you get a big frown and wrinkled brow. When Laura and I talk to him quietly, he looks around, and crinkles a little smile for us.
I had a meeting today with a colleague from out of town who had a similar experience with some very premature twins. It was good to think about something else for a while, and he had good advice for us as an experienced "NICU parent". His big message was to be good to ourselves while we do our best to be attentive to Lukas.
Lesson 5: Pack light. On all of our bike tours, we have been totally self-contained. No sag-wagons to carry our gear, no previously determined routes, no other cyclists. Just me, Laura, two bikes, panniers, and a bunch of maps. We spent 6 weeks in Europe back in 1995 living this way - truly a transformative experience. Of course, other things found their way into our pack: trashy novels (Mark), really erudite intellectural novels (Laura), and the occasional bottle of single malt scotch for emergencies. Since this gear has to be carried up every hill, crag, and mountain on our tour, sometimes covering up to 100 miles in a day, every ounce counts. That means polypropylene underwear, no blue jeans, and only 4 or 5 shirts, 2 pairs of shorts, and 1 set of long pants for 42 days. Our stay in the NICU has shown us that while we love our life in Athens, it is amazing how much of it we could quickly leave behind for the past month. One suitcase full of clothes, one bag of books, and a computer each for the past month, spread out over about 120 square feet of hotel room. A 1 x 3 foot desk for Mark, and none for Laura. Yet, it has been more than sufficient, and we have quickly adapted to this new rhythm. Nevertheless, we look forward to returning to our normal life someday. This weekend we plan to begin "commuting", living in Athens, with one (or sometimes both) of us driving in each day.
Some people have asked if they can share this site's address with friends. We certainly have no objections - we know that putting information on the Web means anyone in the world could potentially see it . That's OK. Laura is keeping a separate journal with more personal thoughts about our stay in the hospital with Lukas.
12/19/2
Lukas had a restful night, with no changes in fluid output or ventilator requirements. His color looked good to us, as he rested on his tummy again. Lukas likes that position for breathing, and they had avoided it for a few days after he had some blood in his stoma, but are trying it again. The liver ultrasound is scheduled for later today - they do that at the bedside. Remember from yesterday that there was some question of where the fluid in his ostomy bag is coming from - is it coming from the stoma (i.e. intestines) or is it leaking around the stoma, where it is stitched to the skin, and actually coming from the ascites in which the intestines are swimming? To resolve that question, Dr. Gauthier will have the nurses put some food color into the feeding tube that rests in his stomach. If the dye shows up in the ostomy bag, then we can assume that the fluid comes from the small bowel rather than the ascites. If not, it probably comes from the ascites and is leaking around the stoma. Lukas also got a new arterial line in the posterial tibial artery on his left foot. The posterial tibial is a small artery just behind the "bump" on the inside of your ankle.
Lesson 6: Keep lines of communication open. When riding, Laura and I always ride single file. We are usually quite close, often within 5 feet, so we can draft. Just like Nascar, cyclists draft to reduce the work for the person(s) riding in the shadow of the lead cyclist. Because we ride so close, we have a series of signals designed to help keep us safe. They include:
- "bump": pothole ahead
- "car back": car gaining on us
- "car up": car ahead of us
- "dive": a bus is coming and we have to dive into the bushes
We're not kidding about the last one - it actually happened several times while biking on a narrow lane in the Dingle Peninsula in Ireland, with a maniacal German tour bus driver bearing down on us. I swear we saw him laugh as we dove into the bushes. Keeping lines of communication open has been important for us during the past 5 weeks. In particular, talking about the things we want to do with Lukas when he comes home (like a bike tour!) helps keep us optimistic about his future. We also make sure we communicate with each of his nurses by being there for part of every nursing shift, and try to spend a few minutes talking to the neonatologist and surgeon at least once a day.
12/20/2
Dr. Gauthier was home sick today; it would have been her last day on the service. Dr. Piazza took over this morning, and will be caring for Lukas during the next 8 days. He took at least 30 minutes at Lukas' bedside to hear the resident's report, examine Lukas, and ask questions, and another hour or two wading through our son's thick chart. (As an aside, doctors will tell you that you never want to be a patient with a thick chart, but our little guy didn't have much choice in the matter.) Dr. Romero, the pediatric liver specialist, also spent at least 2 hours reviewing Lukas' chart and medical history, and also explained his findings to us in considerable detail. We really appreciate the obvious care that both physicians took in getting up to speed with a very complicated little boy, and in spending time answering all of our questions.
Basically, we still cannot be sure what has happened to Lukas. Two key things are going on now: his liver does not appear to be functioning normally, causing fluid in the belly (ascites) and he keeps "using up" his platelets (thrombocytopenia). A viral infection is still a fairly strong possibility, since it can cause both decreased platelets and liver problems. Another possibility is that Lukas has a lysosomal storage disease - examples include Gaucher's disease and infantile sialidosis. Tests are being sent to Philadelphia, where they have the nation's premier children's hospital (CHOP - Children's Hospital of Philadelphia), but they will take two weeks. We hope it isn't one of these conditions, because they are not treatable. The liver looked normal on the ultrasound yesterday, and there was no evidence of blood clot in the liver, but that doesn't help us distinguish between these possibilities. A number of further tests to evaluate his liver function, such as its ability to get rid of ammonia and its ability to make blood clotting factors, are pending.
Below are two of Lukas' nighttime companions - Kelly (left) and Letitia (right). They provide wonderful care for our son when we can't be there, and help us sleep comfortably knowing that he is in good hands. You can see from the photo that Lukas is getting bigger - compare his head with the photos taken while Laura holds him on the first couple days of his life.


Lesson 7: There will be good days and bad days. Some days on a bike tour couldn't be better. The sun is shining, the scenery is beautiful, your legs and lungs feel strong, and at the end of the day you feel like you've accomplished something. It even feels like the entire route runs downhill. Or, to paraphrase the Irish, the road rises to meet your wheels. Other days, it is raining and windy, the route is an endless series of hills, and your butt hurts. Then, you get a flat tire. And a second flat tire. And even (yes, this has happened to me) a third. The only thing that keeps you going is the knowledge that there are more good days than bad, and that if you weren't out there slogging through a bad day, you'd never have the opportunity to experience a good one. As you can tell if you have been reading this journal, the NICU is full of both good days and bad days. Today was harder than most - the news about Lukas' possible lysosomal storage disease was hard to hear. We don't know how likely it is, but have to realize that it is a possibility. We hope that this bad day will be followed by many good ones, and that eventually this time will be but a distant memory.
12/21/2
Just a quick update today. Laura and I drove in from Athens this morning, spent a few hours with Lukas, did some Christmas shopping, and then spent another couple of hours at the end of the day. It is good to sleep in our own bed, see our dogs, and enjoy the company of Laura's parents. Lukas had a quiet day. His vent tube had slipped out a bit, probably because he has been pulling on it a bit. Preemies often keep their hands near their face when they are comfortable, and it is clear from pushing on his tummy that he isn't experiencing much discomfort, which is reassuring. They pushed the tube back in, checked some x-rays, and his oxygen saturation improved considerably. We also had some good news - his ammonia is 114. While this would be high for an adult, it is typical for a preemie, and suggests that at least his liver damage at this point isn't severe or necessarily permanent. A very high ammonia would have been a very ominous finding. We are still waiting for some clotting factor studies, which should be back tomorrow, to give us an idea of how is current liver function is. These factors (5, 7 and 8) break down quickly, so if the level is OK, it means his liver is making them now. Nevertheless, Lukas remains quite ill, though, and it is hard to predict when and if his liver will recover its full function.
12/22/2
Lukas was a good boy last night, and didn't give his nurse Kelly (12/20 photo) any trouble. The big news is that he is now getting a tiny bit of Laura's breast milk through a thin feeding tube placed into his stomach. They are giving 0.6 ml/hour; over 8 hours, that will give him about a teaspoon. While a very small amount, if he tolerates it, they will gradually increase the amount. This is a reflection of his gut (intestines) beginning to work more normally after the surgery. Unfortunately, it does not mean that his liver is any healthier. However, getting nutrition through the gut instead of through an IV (hyperalimentation) is good for the liver, so we hope that this will eventually help his liver as well.
Otherwise, Lukas' heart, lungs, and other systems appear stable. It is hard for his lungs and breathing to improve much given the size of his belly. It is pushing on his diaphragm, so it is as if he were breathing with a big fat guy sitting on his tummy. It increases the work needed, and makes it harder to expand his lungs to an adequate volume. Obviously, if the liver problem resolves, the fluid goes away, and his breathing should improve relatively quickly.
Our friends Allison and Gene were here when I arrived this morning. Lukas gave Allison a finger hug, and his eyes were dancing as he looked up at them. It was very nice of them to take the time to stop by and visit during this busy time. I had a nice visit with Lukas as well, placing my hands on his back and head. He even survived a very scary thing - nursery rhymes. Sung by me. In (gasp!) German. I could only remember one, my favorite, and will have to ask my parents to sing me a few more so I can remember them and pass them on to Lukas. The one I remember is (apologies for misquoting and misspelling to my parents, who taught me German before I learned English):
Fuchs du hast die Gans gestohlen,
Gib sie wieder herr!
Gib sie wieder herr!
Sonst werd dich der Jaeger finden mit dem Schiessgewehr,
Sonst werd dich der Jaeger finden mit dem Schiessgewehr.(Fox, you stole the goose
Give it back!
Give it back!
Otherwise the hunter will find you with his gun
Otherwise the hunter will find you with his gun)
OK, not exactly a politically correct nursery rhyme. Trust me, it sounds much cuter in German! Laura will no doubt find some good vegetarian rhymes for me to sing.
At right is another picture of Lukas, taken today. You can see how his tummy is large in comparison with the rest of his body, because of the ascites. However, his color is good, and he is "filling out" a bit. The yellow tube is the feeding tube that goes into his nose and down into his stomach. The picture is a bit blurry so we can show you Lukas' eyes. It is amazing to me how much emotion and feeling and love can be conveyed by his eyes, even though they are only about a square centimeter in surface area. He dances with his eyes, and we dance with him.

12/23/2
Laura and her father Ken visited Lukas in Atlanta today. His ammonia level, a measure of liver function was down today, which is encouraging. However, the lack of protein (albumin 2.8 today, protein 3.4) and blood clotting problems (his clotting factors are decreased) suggest that he definitely has some liver failure. It is not severe, and we hope that he recovers the function. The great thing about the liver is that it has a terrific capacity for recovery, much better than most organs. Lukas' left lung was somewhat collapsed today, and he is requiring increased support on the ventilator. Hopefully they can get it inflated with increased pressures and changes in position, so he can come back down on his settings. A number of other medications were started today to help him, including steroids for his lungs. He received more platelets and red blood cells today. Our son has had probably 20 or more transfusions during his short life, and has almost certainly had the equivalent of his entire blood volume replaced a couple of times. Most people never have even one transfusion during their lives. There is no sign of infection, and a whole slew of tests for rare, awful conditions were sent out today.
Dr. Piazza spent a lot of time coordinating Lukas' care today, working with the pediatric hematologist (newly consulted), pediatric hepatologist, laboratory, nurses, ostomy nurse, and pediatric surgeons. Lukas was a busy boy today, and seemed to be tired and a bit out of it. Hopefully he'll have a better and quieter day tomorrow. Perhaps the best news is that he tolerated his feeding with breast milk well today, and they will hopefully be able to tweak the rate up a bit tomorrow.
My parents Herbert and Hildegard drove up from Florida for the Holidays, and will be staying here till Thursday. It's great to see them, and we had a wonderful dinner with both sets of parents at DePalma's, our favorite Italian restaurant in downtown Athens. It was the first place Laura and I ever went to dinner in Athens and remains our favorite.
12/25/2
Sorry for the lack of an entry yesterday - the MSU server was acting up a bit, and I needed a day off anyway. My parents joined me in visiting Lukas on Christmas Eve, which was nice. He even squeezed my mother's finger, a memory I'm sure she'll carry back with her to Florida. Today, Laura and I visited Lukas and spent the afternoon with him. We had some nice interactions, as you can see below. He had another visitor this morning - Santa stopped by! We'll scan the picture in at Laura's office when we get a chance, it is just too cute.

You can see from Lukas' picture that Santa left behind a little replica to keep him company. You can also see that Lukas looks puffier - he now has a truly Churchillian double-chin. His belly looks a bit smaller to us, though, although it is hard to be certain. His blood protein levels are creeping upwards a bit, which is good. His albumin is now 3.7, up from 2.8 the last time it was measured. His urine output is also good, at 4.7 ml/kg/hr, which is quite a bit. We hope that the albumin is drawing excess fluid into the bloodstream, and then the Lasix (a diuretic) is helping him excrete it. His ventilator settings have been fairly stable for the past 24 hours. We had some scary moments yesterday when he was requiring 100% oxygen and still not getting enough, particularly when he got excited. While he could go back on the oscillator if he had to, we'd obviously like to avoid it.
We both agree that we are an odd place mentally. Laura and I have spent our entire lives planning ahead, making lists, and being very goal oriented. Probably to a fault - it is almost impossible for either of us to just sit around and do nothing. That is why golf has been such a wonderful release for me - it is a chance to be outside, with friends, doing something I enjoy, with no possibility to work. With Lukas, we are forced into a day by day existence. Part of that is that his condition fluctuates so much from moment-to-moment, but part is that we don't want to allow ourselves to look too far ahead. We don't want to dwell on the worst, but we also don't feel like we can allow ourselves to get our hopes up too high, lest we crash down at some time in the future. Thus, day to day is best for now.
Special thanks to his nurses (Monica, Kathryn, Jody, and Kelly), respiratory therapist (Lester), and physicians (Drs Mohommed, Dr. Piazza, and Dr. Sexton) who took care of Lukas on a day when I'm sure they would all have rather been with their families. We appreciate your sacrifice very much.
One of the presents we got is a tape recorder and tapes for Lukas' bed. We hope to record our voices, talking to him, reading books, and even (here's the scary part) singing. Hopefully Lukas will be well enough in the next week or two that we can begin to do that for him.
12/26/2
Lukas Willem Bierema Ebell, our son, our love, our prince, died today as we held him in our arms. The phone call we were dreading came at 5:30 in the morning from the neonatologist on call, Dr. Sexton. He said that Lukas was having more trouble breathing, with his belly increasing in size, his carbon dioxide level going above 100, and increasing difficulty maintaining an adequate level of oxygen in the blood. To take the pressure of his lungs and help Lukas breathe better, the neonatologists decided to place an IV catheter in his belly to draw some of the fluid off. Toward the end of the "tap", a small amount of blood was seen. Later in the evening, it was clear that he had been bleeding into his abdomen. Lukas was very pale, and his lower abdomen and scrotum were a bluish color from the blood. That is when we were called. By the time we arrived about 90 minutes later, the nurses and doctors were doing their best to keep Lukas alive. His blood pressure when we arrived was only 15/10. Normal for an adult is 120/80, and normal for him as been about 54/26. This very low blood pressure for two hours or more almost certainly damaged his brain. Unfortunately, there was nothing they could do to increase the blood pressure because he was bleeding so quickly. They tried to withdraw fluid again from his belly, but this time got only blood. Lukas' liver disease was so bad that his blood did not clot normally. He has received many transfusions of platelets, red blood cells, and fresh frozen plasma, and had several of each today, but to no avail. He would not stop bleeding. Despite this, our little Lukas looked around at us with his beautiful, blue eyes. He never looked more beautiful to us.
We had two heartfelt conversations with the health care team, who helped us understand that Lukas' situation was becoming more futile, and that the options for treatment were very limited. Then the two of us talked. Our goal for Lukas was always that he be able to come home with us and be able to interact with us and others in a meaningful way. Appreciate a sunset, smile at a puppy, and laugh at a joke. Because of the high likelihood of brain damage caused by his underlying illness, the near certainty of brain damage from the bleeding and low blood pressure today, and the very low likelihood of recovery in any way from his illness, we decided to withdraw care. The nurses turned off his IV fluids, disconnected as many lines and leads as possible, and dressed Lukas in a beautiful blue gown, cap, and booties. They gave him some morphine to calm him, and keep him from becoming short of breath. We both cradled Lukas in our arms, and while he still had his eyes open, by this time he seemed to be staring off into the distance. When we said we were ready, the nurse gave him some Versed, a medicine to calm him, and the doctor removed his ventilator tube. Lukas' strong heart gradually slowed, and his breathing stopped. He passed from us at 11:40 am.

Lukas has touched many lives, none more so than our own. We believe that Lukas taught every one of us important lessons. We believe that Lukas loved us, and that we loved him. We believe that he felt pain, but is no longer suffering. We believe he knew us and loved us as we loved him. We believe that we will carry his fi
erce desire to live with us till the day we die. We believe that every life is sacred and meaningful, no matter how short. We believe that our beautiful little boy is finally at peace.
If you would like to honor Lukas' memory, we have established a non-profit organization called "Lukas' Fund". We plan to work with the nurses, therapists, and doctors who took care of Lukas to identify the needs of the neonatal intensive care units at Grady Hospital in Atlanta. They will tell us how to spend the money. Our focus will be on touch, not tech. Possible purchases include special gel pillows for baby's heads, preemie diapers, educational materials to help parents interact with their premature child, bedding materials to assist in positioning, and books or videotapes on parenting for the waiting room. Grady Hospital had none of these things for the preemies, and we know that Lukas would want to do anything he could to help his "roommates".
Thanks to all of the nurses, respiratory therapists, physical therapists, physicians and others who helped care for Lukas during the past 6 weeks: Kelly, Kathryn, Kathleen, Leticia, Jill, Melinda, Monica, Connie, Peter, Lester, Janice, Danali, Marie, Ted, and Drs. Faase, Goggin, Biddle, Dudell, Gauthier, Schaeffer, Sola, Sexton, Piazza, Romero, Pettit, Bullock, Mohammed, and Parker, and all of the others whose names we may have forgotten but whose love and care attention we have not.
12/30/2
We would like to thank all of you who have called, stopped by, written, or emailed us to express your condolences. We miss Lukas very much, especially when we imagine him as he would have been, taking part in our lives. We are trying to get back to those lives now, and look forward to seeing all of you and giving you a big hug in the near future.
Lukas' memorial service will take place at 4:00 pm on Wednesday, January 8th at the Day Chapel on the grounds of the State Botanical Gardens in Athens, Georgia. It will include thoughts and prayers from friends and family, photos of our son, and a brief reception afterwards. You can follow links to learn more about the Day Chapel and to get directions. We look forward to seeing you.
A Memorial Service was held on January 8, 2003 at the Day Chapel the State Botanical Gardens of Georgia. Laura and Mark's remarks at the service are excerpted below.
January 8, 2003
Dear Lukas,
Our time with you was too short. We wanted the chance to get to know you. We wanted to be your parents through infancy, the so-called terrible twos, awkward adolescence, and on to adulthood. We wanted to know the worry, aggravation, and joys of being your mom and dad, and did for a short while. And yes, we even looked forward to the times you would roll your eyes in exasperation at us—your parents. Your dad wanted to teach you to ride a bike, build a model, and swing a golf club. I wanted to relive childhood through your eyes and teach you to be a feminist. We wanted to take you to Manistee to acquaint you with sand, sun, wildlife, and sunsets. We dreamed that you might grow up to be a neonatologist, to help other children who had a rough start in life, just like yourself. Well Lukas, all those hopes were not to be.
We think about all the things you never had a chance to do. To see the sun, to breathe fresh air. To read a book, run through the woods, or swim in Lake Michigan. To make a fuss in a restaurant, or watch a movie in rapt attention. Just to sit up, look at us, and smile. As we try to get back to our lives, though, Lukas you are with us. When I’m driving, I imagine you in a car seat behind me, watching for a big truck. As I play golf, I imagine you standing there, wincing at my mis-hits and laughing. As the dogs play, we imagine you tantalizing them. As I walk by your room, I imagine that I hear your cry. You will always be with us.
Lukas, we love you deeply and miss you intensely. Your body may have failed you, but your fierce spirit and will to live are alive in our hearts today. Your courage, will, and dancing eyes amazed us. You made it clear you wanted to stay here. Your dad and I believe that your life was sacred and special and important. But we don’t think that you were put here just to teach a few adults some lessons through your suffering. Your purpose, to grow and live and love, was unfairly interrupted. Still, I can’t get beyond the fact that you are the smallest, youngest, and most powerful teacher I’ve ever met. As Ralph Waldo Emerson observed, “Death puts Life into perspective.’’ You have certainly given us perspective Lukas, so, in this letter, we want to tell you what you taught us, and what you continue to teach us each and every day.
You taught us that life is random, and chaotic, and sometimes awful. We can’t understand why our beautiful son, who was so loved, and would have had so much to offer the world, died. Your mom and I have never been in a situation where we couldn’t succeed by simply working longer, working smarter, or working harder. Your illness humbled us. All we can do is try to create meaning where there appears to be none. Your lessons were many. You taught us that balance is important, that rain stops, and to pack light. You reminded us of the importance of good communications, but that sometimes it is best to keep ones mouth shut. You helped us understand that there will always be good and bad days. Your final lesson was that some hills are just too high to climb.
You taught us that love happens fast. We fell in love with you instantly. We will always have a special place in our hearts set aside for loving you Lukas. You taught us that “Patience is also a form of action.” We saw this Auguste Rodin quote scrawled on a chalk board in a restaurant one night at dinner when we were deep in despair. You must have been sending us a message. With each passing day, you showed us that if we were patient things would get better, and they did for awhile. Now we focus on being patient with our grief and accepting a life without you in it. You also showed us how suffering can happen with grace. Lukas, you suffered more in 6 weeks than most people will in a lifetime. Even though you were in pain and sick, you were happy to see us and greeted us with dancing eyes and finger hugs.
Lukas, you taught us to never take anything for granted. If you could, I’m sure you’d tell our friends and family to hug their children, kiss their partners, make every moment count, and not to worry about the trivial or mundane. Your body is now ashes, to be returned to the earth. You would want us all to hold that earth and sky and water sacred, to walk in the woods, ride a bike, plant a tree, and savor a sunset.
We both wonder where you are now. We don’t believe in the notion that heaven is a place full of harps and angels in white robes up in the clouds. But we also know that our knowledge and wisdom are incomplete. You had a special, strong, energy in those eyes, that heart, that mind. We believe that this energy did not just disappear, but rather that it is now part of what binds us to one another, and brings all of us together today to celebrate your life. Heaven is what we create with our love here on Earth, and you are part of that.
Lukas, we don’t understand why you were born so small and so sick. We are sorry you were too sick for us to hold you and that we could not kiss your sweet face until you lay dying in our arms. I am sorry I never heard you cry, or talk, or sing. I loved staring at your beautiful, perfect face, long graceful fingers and reddish locks of hair. I loved gazing into your deep blue eyes when you were awake. I loved watching you sleep comfortably in your incubator. We are thankful that we could share tender moments, exchange finger hugs, cradle your head and feet in our hands, and dance with your beautiful blue eyes.
And did those eyes ever dance! You knew when we were there, you knew your favorite nurses, and we could tell when you were happy and when you were sad. We also knew when we got the call at 5 am that final day that you were very, very sick. Yet when we arrived, despite having almost no blood pressure, your eyes opened, and you welcomed us. Your big, beautiful, blue eyes looked from side to side, and danced with us one last time. You were saying goodbye in the only way you could. And I finally had a chance to hold you, and feel your weight. Cradle you, and kiss you, and cry.
Lukas, we will always be your parents and you will always be our son. On December 26, your spirit left your body, but not this world. We will carry your spirit with us and know that it will remind us to love each other harder, work less, act with patience, shed the petty and unimportant, share your gentle presence, and to be strong and courageous like you.
We love you,
Love,
Mom and Dad